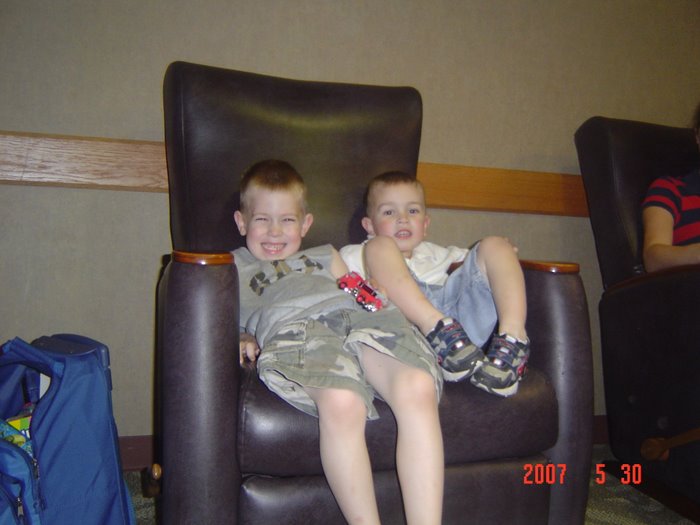
And we did have a nice one. I didn't make it out of the hospital to shop, so Josh got a Riley t-shirt (actually thinking about getting one myself) some nut goodies, and some cherry sours - yes, they are his favorites! I also had the boys draw him some pictures, while he was over at the hospital having an evening visit with Gabe. I told him he could choose where to go eat for lunch and he chose Chuck-E-Cheese! Ok, he's a better paren than I am. I wouldn't choose that particular restaurant on Mother's day (Hmmm... makes you wonder who the biggest kid is!)
Although I
did take the boys to see The Wiggles Live last year on Mother's Day,
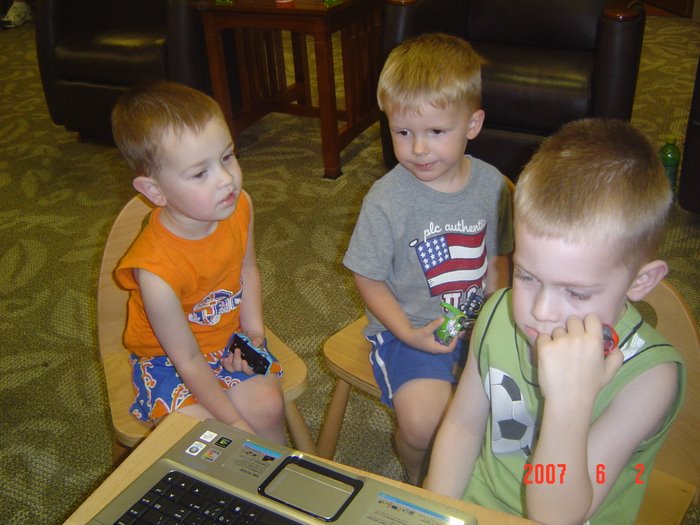
without Josh. Surely that is one of the requirements for sainthood - or it should be. While I was watching the boys having a great time playing air hockey (all three of them) I couldn't help but think how much fun Father's Day will be next year, with Gabe probably attempting or perfecting his first steps. I love watching those first wobbly staggers, which usually end in crashes!
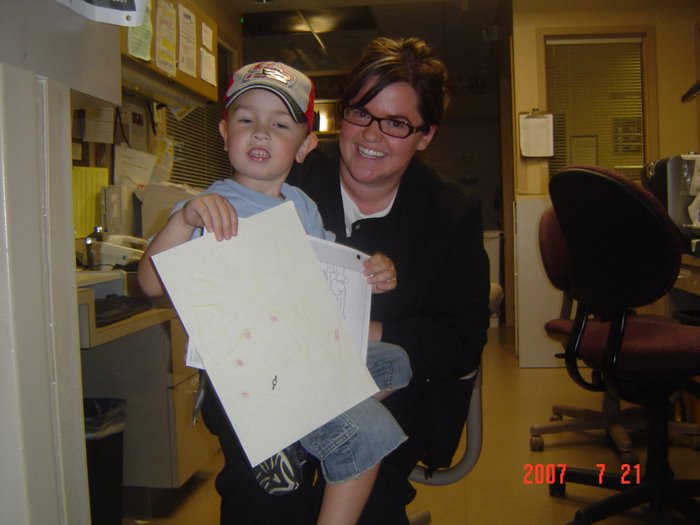
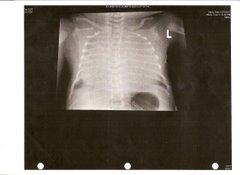
Gabriel made a nice card for Daddy too, it was sitting on a shelf by his bed when we got in there today. I'm sure the nurses helped him, at least a little bit. Speaking of Gabe (he is the point of this blog, after all) he had another steady night. They haven't really weaned him too much more from the ventilator, maybe b/c of the slight right pneumothorax, they didn't really say. Another chest x-ray was done this afternoon with Gabe on his side so they could see the right lung better. Our understanding is that they still aren't too concerned about it, just keeping an eye on it. The left chest tubes are still putting out very little (let's hope the pleuradesis worked!) and the right is staying about the same. I'd imagine that if that does not change soon, we'll be back in the OR for lung scraping on the right. I suppose if it works, it'll be worth it.
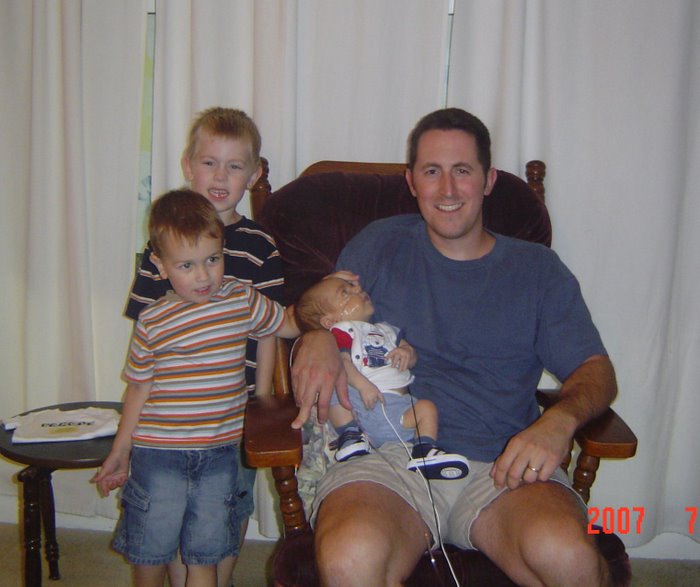
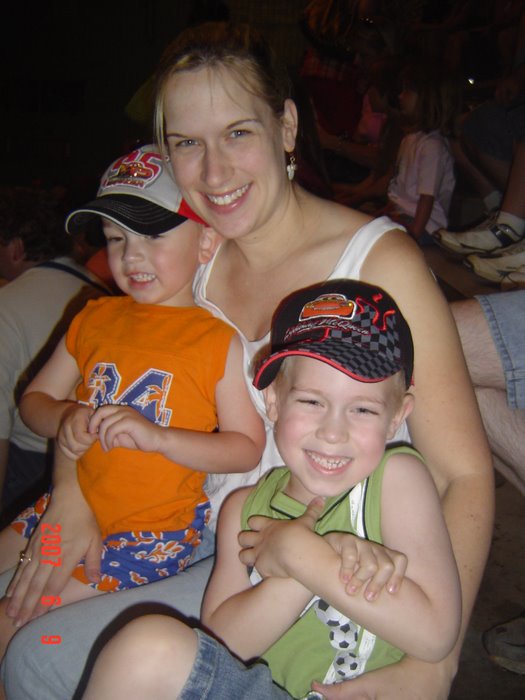
Gabe had his eyes open quite a bit yesterday and we got some good pictures of him with the boys. Deb, one of our regular day nurses, got a picture of all five of us with Gabe's eyes open. I also got a picture of Tabatha, who is a regular night nurse. They are all posted below, along with Father's Day pics. If I haven't mentioned it lately, thanks again for all of the posts, cards, emails, and calls. We continue to appreciate the support. Every time we talk to our family, they let us know about somebody else who reads the blogs daily, and that is very touching to us - to know that so many care about Gabriel and us. So, thanks!